Being on blood thinners
What is a Being on blood thinners?
Blood may clot in a critical point, resulting in loss of blood supply and death of an organ. If diagnosed in time, the doctor advised you to remain on long term anticoagulation, to prevent this from happening. The usual scenarios where this is considered are
- A coronary stent has been placed recently
- There is an artificial heart valve recently placed
- There has been a clot in the veins, with a risk of spreading to the heart
- There is atrial fibrillation, and so a risk of clotting in the heart itself
It is critical that the blood is neither too thin (risk in bleeding), nor near normal (risk of clotting).
If some digestive disease becomes a cause of bleeding, there is a risk of prolonged bleed as the blood will not clot. There could be a justification for a monitored discontinuation of the anticoagulant, balancing the risks of bleeding with the risks of a vascular event. It is thus important for you to know every aspect of the reason you are on anti coagulants. It would also be good to have a summary of how your anticoagulant management has progressed since it was started.
The summary should include
- The cause of being on a blood thinner,
- The name and contact details of the doctor looking after it;
- Blood reports showing the doses that are being used to maintain a stable drug level & and
- The anatomical diagnosis and status for which this has been planned.
- Other medications that are being used concurrently
Whenever you are going for any health related visit to the hospital, whether it is a routine or an emergent cause, even for a test; this information may be sought, and you may need to produce all details at a short notice. You could
- Save a soft copy on your Drive in the mailbox, or the cell documents
- A hard copy may be the first page of your health file.
- Copies should be with your care givers too
What can be called the “Perfect Preparation” for a colonoscopy?
For your doctor to see the bowel wall clearly, the bowel needs to be completely empty. To help clear itout you will be asked to follow one of two protocols, if you want a fautless procedure The first involves drinking two liters of a solution of polyethylene glycol (Peglec or Colopeg) that causes temporary diarrhea. It comes in 2 flavors, which, unfortunately, only partially mask a somewhat unpleasant taste. Refrigerating the solution may make it more palatable. Drinking such a large volume of cold solution may cause a patient to feel chilled, but the sensation is temporary. Do not add flavoring (additional sugar or salt) to the solution. Many patients say that drinking the purgative solution is the most unpleasant part of the examination!
I usually prefer to ask patients to make the solution the night before; so they will not lose time making it when they wake up. You could drink it in two hours about 4 to 6 hours before the scheduled time for the test; at the rate of a glass (200 ml) every 10 minutes. In case you feel nauseous, slow down, so you do not throw up and need to start with a fresh two liter solution all over. You will pass about 5 to 8 watery stools, the last of which are expected to be the color of the solution you drank.
The second method involves drinking a solution called Exelyte (2 bottles of 45 ml each in a box) mixed in 300 ml lime juice or Limca over half an hour, followed by several glasses of fluids. This preparation is easier to consume (just 2 glasses of a juice, each over 15 minutes) than the Polyethylene glycol.
However, Exelyte is a cathartic; it makes you loose body water to make loose stools and you should be careful not to get dehydrated. I prefer to check that you do not already have a borderline renal damage (do a Blood urea & creatinine test); else giving this solution and not hydrating later may aggravate the kidney damage. It also contains a large amount of phosphorus, which may be a problem for people with heart or kidney conditions. It is very important that you drink frequently throughout the day to avoid dehydration. Drink water, soft drinks, fresh as well as canned juices, chicken or vegetable soups, coffee or tea (no milk; sugar is fine). Avoid foods with seeds the previous day (brinjal, guava) as well as supari & saunf; it remains undigested and then clogs our scopes!.
What to Wear
Please wear loose, comfortable clothing. Please leave your valuables at home. Wear comfortable, stable
shoes since you may be a little unsteady when you leave. You will be changing into a patient gown
before the procedure.
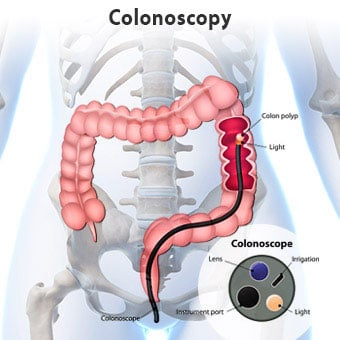
What actually happens in Colonoscopy?
With you resting on your left side, your doctor will gently examine your back passage with a gloved
finger & lubricating jelly before carefully inserting the colonoscope. Air is then usually passed through
the tube into the colon to make it expand and the bowel wall easier to see. This may briefly cause pains
similar to having wind and you may get an urge to go to the toilet, but as the colon is empty, this won’t
be possible.
Most people pass some wind. There is no need to feel embarrassed about this as your doctor will expect
this to happen. During the procedure, you may be asked to change your position – for example turning
from your side onto your back. This helps your doctor to examine different areas of the colon more
easily. If necessary, your doctor will take a biopsy and/or remove polyps. This is done using special
instruments passed inside the colonoscope, and is quick and painless.
I would prefer sedation for the procedure!
Our Anaesthesia team will make sure you are comfortable throughout the procedure. It would be
preferable for them to review your records in advance, so they can plan appropriately for the day of the
procedure. The sedative will be injected through the cannula placed in the back of your hand, and you
should start to feel relaxed and drowsy almost immediately. Sedatives can sometimes affect your
breathing, so the amount of oxygen in your blood will be monitored constantly through a clasp on your
finger and you may be given extra oxygen through a mask.
After your procedure is complete you will be taken to the recovery area. The nurses there will continue
to monitor your blood pressure, pulse and oxygen saturation. Your “significant other” or friend may
come sit with you in recovery at this time. You may need to stay in the recovery area for even up to
three hours. Plan so you do not need to drive, operate machinery, sign any important documents or
make important decisions until the next day. You should not exercise strenuously until the next day.
You must make arrangements for a responsible adult to drive you home after your procedure. Taxis and
buses are not permitted unless you are accompanied by a responsible adult.
