ERCP
What is ERCP?
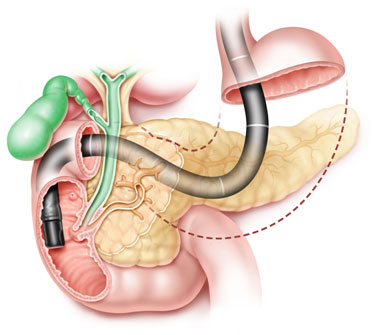
As food gets digested in the stomach, it moves down into the first part of the intestine (duodenum),
where digestive juices made in the liver and the pancreas are poured over it. These juices are sent down
to the intestine through tube like ducts. Bile made in the liver is stored in the gall bladder & travels
down through the Common Bile Duct; the pancreatic duct is the drainage route of the pancreas. Both
these ducts (tubes) open into the intestine at an opening called the Major Duodenal Papilla.
ERCP (Endoscopic Retrograde Cholangio Pancreatography) is
- a specialized endoscopic procedure
- that accesses the ducts from the papilla backwards (retrograde),
- gets information of the liver, gall bladder and bile ducts (cholangiogram) and
- the pancreas (pancreatogram).
Are there any risks in the procedure?
ERCP is a well tolerated procedure when performed by doctors trained & experienced in the technique. Complications requiring hospitalization are uncommon. These may include pancreatitis (inflammation of the pancreas), infections, bowel perforations & bleeding; which are however, rare. Some patients may get an adverse reaction to an antibiotic, sedative or radiologic dye. Sometimes the procedure may not be completed due to technical difficulties. The risks vary, depending upon whether the patient already has major medical problems, and the degree of difficulty in the therapeutic intervention planned. Your doctor will be able to tell you what the risks are in your specific case.
For which symptoms is ERCP commonly offered?
Obstructions to the bile ducts due to stones slipped from the gall bladder, or due to cancerous growths of the gall bladder, bile duct & pancreas block the flow of bile resulting in jaundice. If infection sets in the stagnant bile it can progress rapidly with life threatening consequences. Blocks in the pancreatic duct can also happen due to pancreatitis or tumors, resulting in severe constant pain. ERCP can identify the cause & precise level of the block, as well as give an access to relieve the obstruction too. Suspicion of these diseases is made during ultrasound or CT scan examinations.
Are there any alternatives to ERCP?
Visualization of the bile & pancreatic ducts is now possible by MRI techniques called MRCP. Thus, MRCP is an alternative if being done for diagnosis alone. ERCP has a reasonable accuracy for obtaining tissue to confirm presence of cancer, which MRCP cannot give. If a patient has a confirmed cancer that is operable for cure, your doctor may suggest you see a surgeon right away and not have the ERCP at all. Removals of bile duct stones by ERCP are now standard-of -care procedures; meaning the alternative of removal by surgery is accepted to be more morbid. Every problem ERCP addresses has previously been offered a surgical option. For your specific abdominal disease & co-morbid conditions, your doctor will be able to tell you what the relative risks & benefits are, between ERCP and surgery.
How is ERCP done?
ERCP is usually done after admitting the patient indoors. Your stomach should be empty so you are advised an overnight (or at least 6 hours) fast, else you may aspirate the gastric contents into your lungs leading to a pneumonia. . You are likely to receive an antibiotic before the procedure, so inform your doctor if you have allergies to any drugs previously.
If the procedure is likely to be lengthy, your doctor may plan conscious sedation; so you are unaware about the procedure, but your basic reflexes are intact. Rarely is full anesthesia required. You should tell your doctor in case you are using medication for major chronic ailments (like diabetes, blood pressure, heart or lung disease, arthritis, etc.) as he can take appropriate precautions.
A duodenoscope is passed from the mouth into the duodenum till the doctor sees the common opening of the ducts of the liver & the pancreas. The instrument does not interfere with your breathing, but there may be a bloating sensation if your doctor needs to pass air to have a clear field of vision till the Common Duodenal Papilla is seen. A narrow plastic tube (catheter) is passed through the duodenoscope into the ducts & contrast material (dye) is injected so the ducts show up on X-ray screens. Please inform your doctor if you have had previous radiologic procedures involving injection of dye, and had an untoward reaction to it. Once the problem is identified, the mouth of the papilla is widened with a cut, so larger treatment devices can gain access into the duct. If you are using aspirin, or blood thinners (clopidrogel, warfarin, etc) tell your doctor well in advance, so he will take appropriate precautions to prevent a risk of bleeding. At the end of the procedure, a thin plastic (Teflon or Polyurethane) tube is left where the ducts were entered. This is because handling of tissues causes swelling and may block the ducts. This tube (stent) allows free flow of digestive juices till healing is completed by the body around it.
The stent is an artificial device; it can get blocked within 2-3 months. Your doctor will thus need to re assess you by duodenoscopy within this period for removal. In some patients, permanent relief from obstruction to bile ducts due to tumors can be done by placing SEMS (Self Expanding Metallic Stent). This is usually offered to those patients where the obstruction is confirmed to be due to a cancer; & surgery for the tumor is unlikely. These stents will not need to be removed as they are not associated with a risk of infection & blockage. Following the procedure, you may need to remain indoors for between 6 hours to 4-5 days, depending upon the severity of the problem you are being treated for.
