Liver cirrhosis
What is Liver Cirrhosis?
What is Liver Cirrhosis?
The natural response to organ injury in organ repair. If the injury is short & simple, the repair looks as if the injury never happened before. In case the injury is repetitive and constant, there is a struggle to repair, thus more scar tissue is laid down resulting in a distorted appearance. Distortion results in a reduction in efficiency of the remnant liver. This is the essence of understanding cirrhosis.
Cirrhosis is inflammation of the liver that has been going on for a long time. Prolonged injury causes scarring in the liver, as well as the destruction of the liver cells; thus reducing the ability of the liver to function efficiently. Unless the cause of cirrhosis is removed, this liver damage may gradually progress; leading to more deterioration in function. Following is a brief outline of how a normal liver functions, and what could happen in cirrhosis.
Here, let’s understand why a person with liver cirrhosis may get the following symptoms
- Vomiting of blood
- Weight loss
- Abnormal blood clotting
- Swelling over the feet and collecting fluid in the abdomen
- Sometimes get disoriented
- Get repeated infections
- Have itching & jaundice
- …but all this could reverse, too.
• Cirrhosis means the liver has become ‘hard’
The food we eat is broken down in the intestine and absorbed into the blood after which, it is brought to the liver by the portal vein. The blood flow coming from the intestine easily percolates into the liver like a sponge, so the liver cells can quickly deal with the digestion.
In cirrhosis, the liver is scarred; so it gets hard. The blood from the portal vein cannot reach to the each part of the liver quickly & properly. Blood backing up may cause distension of blood vessels in the food pipe. If the back pressure rises too much, the vessels may become very thin and rupture. This results in vomiting of blood.
Cirrhosis means the liver cannot manufacture:
The liver decides how much food should be used immediately, how much should be stored for later use; and what should be converted to proteins (the building blocks for muscles and other tissues). Glycogen (complex sugars) and long-chain fats are storage forms of sugars (in the liver & muscles) & fats (in the abdomen & under the skin) that occupy less space.
In cirrhosis, the liver cannot handle the demand & supply of energy. As it cannot keep up with the demand of making proteins, patients experience weight loss, lose muscle mass and look emaciated. Sugars are needed as ready energy for the brain; lack of prompt supply of sugars when needed makes a cirrhotic weak & tired earlier than usual.
Manufacturing of proteins- the liver provides building blocks for making muscles and tissues. It also makes clotting factors needed to seal off the bleeding points.
In cirrhosis, clotting factors are deficient; so if bleeding starts, it may not stop easily.
Albumin in the blood maintains the “oncotic pressure” in the bloodstream; this ensures that the water from the ‘thicker blood’ does not flow out into the tissues.
If there is a shortfall of albumin too, then oncotic pressure cannot maintain in the blood, and water escapes. This collects as fluid in the abdomen and swelling of feet.
Cirrhosis means the liver cannot remove dirt:
The liver can identify, break down and dispose of the waste. Ammonia is one of the waste products generated by protein breakdown and is disposed of by the liver.
If the removal of ammonia from the blood slows down, high blood ammonia may cause a cirrhotic to appear confused, or even lose consciousness (encephalopathy).
Bile acids are secreted in the bile which is poured onto the food entering the intestine. Bile acids are needed to break down fats so that enzymes can effectively digest and then absorbs them. Bile pigments (bilirubin) are a waste product cleared by the liver into the bile.
Bile contains bile acids, which break down fats in food. Inability to remove bile acids into the intestine may cause a cirrhotic to get itching. Bile pigments (bilirubin) are generated as waste products and if the liver cannot filter it out of the blood it will result to jaundice.
Cirrhosis means the liver cannot fight infection:
Immune defence – Along with the digested food, many germs enter the blood from the intestine. As the blood from the portal vein enters the liver, the white blood cells and R.E. system filters the bacteria but allow food to pass through into the liver cells. In addition to clearing the blood coming from the gut, the liver also clears the general circulation of bacteria, if any.
Severe alcoholic hepatitis can impair the liver’s ability to clear gut bacteria. In addition, having a damaged liver may allow repeated infections anywhere in the body. Normal people may clear simple infections on their own; or need oral antibiotics; – in cirrhosis patients may require hospitalization for simple complaints.
The liver can get damaged, but it can recover too
Signs of liver disease could start showing when a lot of liver tissue has failed. All patients may not show all the signs of liver disease; some may only have to bleed; whereas some may only have a collection of water in the abdomen & swelling over the feet. The liver has tremendous power of regeneration. Removal of the cause of liver damage sometimes leads to regression of cirrhosis.
How bad is my Chronic Liver Disease?
Often the question is asked “How much is my liver damaged? Is it 50% damaged – or 80%? Is it “failed”? How the doctor will like to explain the situation is by the risk that liver cirrhosis is to your life.
Cirrhosis makes your liver functionally smaller:
You need to understand is that the liver has many functions – it clears waste, it makes protein, it detects and clears germs from circulation, etc. Assume that you have been given more than 100% capacity of each of these functions. That is, you need some function to get along in normal life; and you need plenty of reserve to deal with a crisis.
In cirrhosis, this capacity starts reducing. Your liver may not have a reserve when faced with a crisis. Let’s say, you suffer a bout of malaria; or you need to be hospitalized for a broken leg. In a situation of increased demand, your health may collapse suddenly; as the liver may not be able to clear waste, make protein fast enough to repair; or clear infections. In such persons, trivial infections that usually get better with treatment at home; need ICU care for survival.
Doctors call the stages of a “dropping liver reserve” are as follows:
- Compensated cirrhosis
- Decompensated cirrhosis
- End Stage liver Disease
Compensated Cirrhosis:
Outwardly, you may appear completely normal. There is a 99% chance that you will not have any adverse liver related event in the next year, the figure drops only to 97% if you also have had varices in addition. You may be leading a perfectly normal life; and your liver is providing for the regular day-to-day needs. You still need to be careful. You have a median survival is 9 to 12 years; with a rate of progression to decompensation at 5-7% per year. Screen for enlarging varices to prevent bleeding.
Decompensated Cirrhosis: clear cut complications of liver cirrhosis are now apparent, so also are the chances of a risk of death. Having detectable ascites as well as varices raises the risk of death from another complication in a year to 20%; if the varices have bled; this will be 50%. Other complications are having jaundice, encephalopathy and other hepatic insufficiency. This is the time when you are suggested to be evaluated for a Liver Transplant.
End-stage-Liver-Disease: the disease is so advanced that you need frequent in-hospital care for survival. Liver Transplant is an obvious choice; however, the immediate outcome as well as recovery from the procedure may not be as smooth.
How much of my liver is damaged?
All along, your liver doctor wants you to recover whatever liver you have lost, bit by bit. This is a long journey. You may be progressing well; but, God forbid; if you fall sick, you will lose whatever you have gained. You will want us to tell you what the chances of a good outcome are in case you fall sick.
There are various scores doctors use to predict outcome in your life in the state you are in, in case a crisis comes along. Calculating a score makes it easy to judge what the outcome would be in case you suddenly fall sick tomorrow. The commonly used scores are:
- CTP score (Child Pugh Turcotte)
- MeLD score
These scores use the blood values of bilirubin, albumin, INR and creatinine; and clinically evident ascites and encephalopathy. A gradually rising score over time means you are not doing well at all and you may be safer with a new liver. UNOS (United Network of Organ Sharing in the US) as well as Eurotransplant use these scores to prioritize allocation of available donor livers. Studies have found that mortality rises as the MeLD score rises, and chances of survival for 3 months is as follows
MeLD =/> 40 3% mortality
MeLD 30-39 6% mortality
MeLD 20-29 6% mortality
MeLD 10-19 0% mortality
MeLD < 9 9% mortality
Anywhere in the world, a liver doctor will only look for the MeLD score and CTP score then answer the question “how much is the liver damage”.
How frequently should I be doing my Liver tests?
Because the mortality rises, a liver doctor will need to see you earlier if the MeLD score is higher. In the US, to remain on the transplant list, for a previous MeLD score, you are needed to update your current lab values as follows:
- MeLD > 25 blood reports every 7 days
- MeLD 24-19 blood reports every 30 days
- MeLD 18-11 blood reports every 90 days
- MeLD 10 blood reports every year
What are complications of Liver Cirrhosis?
When the doctor uses medical terms to describe complications, you will need to know more what they are.
- A tendency to bleed (Impaired clotting of blood)
- Vomiting of blood (Portal hypertension and varices)
- Collecting fluid in the stomach (Ascites)
- Disorientation (Encephalopathy)
- Deteriorating kidney function (Hepatorenal syndrome)
- Breathlessness (Porto pulmonary syndrome)
- Bone pains (Ostoporosis)
- Muscle loss (Sarcopenia)
- Liver cancer (Hepatocellular cancer)
Portal hypertension and Gastro-Intestinal Bleeding
The liver receives blood supply from 2 vessels, hepatic artery and the portal vein. The hepatic artery is bringing in the oxygen, & the portal vein is bringing blood from the intestines, which means, it contains all the nutrition that you are attempting to get from your food. Both are important to nourish the liver. Blood soaks into the liver tissue and exits to the heart within 6-8 seconds. When you get cirrhosis, three things happen:
- The liver is not as soft a sponge it should be; and it is progressively more difficult for the blood to soak into the liver tissue. If the cause of the liver damage is not corrected, the liver will become progressively tougher to penetrate, increasing the resistance on the feeding blood supply.
- Thus, in the veins, blood will back-up; and, like the backwaters of a dam, will put pressure on blood vessels downstream. Veins start enlarging in the esophagus (the food pipe, thus called esophageal varices), where they may rapidly get thin-walled with a consequent fear of rupture.
- The cirrhotic liver is surviving more on the blood supplied by the portal vein than the artery. If you fall and loose a liter of blood from your arm or leg, there will be an average impact on all organs in the body. Bleeding from branches of the portal vein steals nutrition from the liver itself. Thus, 10% to 50% patients may die from an episode of bleeding.
When your doctor diagnoses you as having Liver Cirrhosis, one of the aims of his treatment, is not to let you bleed, thus, —
- To detect esophageal varices,
- Prevent them from enlarging (pre primary prophylaxis),
- Blocking them off if they do enlarge (primary prophylaxis), and
- Keeping a regular check to see they are not returning (surveillance).
If the Liver cirrhosis was diagnosed after you bled from varices; there is a 30% chance you will bleed again in 6 weeks & 62% chance in the next 2 years. Thus, the doctor will keep rescheduling you for endoscopic treatment till all veins have disappeared (secondary prophylaxis).
Endoscopic treatment to prevent bleeding is usually done as a ‘day care’ procedure, when you could be sent home in the evening; on the other hand, the hospital stay after you have bled could be anywhere between 4 days to 2 weeks, and cost between 4 to 10 times the cost.
Bleeding from varices of portal hypertension is not like any other bleeding in the gut.
- The chances that you may die of a single “bleed event” are high; especially if you have advanced liver disease (CTP C – 33%, vs CTP A-nil, B-10%), or you have comorbidities like alcoholic hepatitis, sepsis, organ failure, portal vein thrombosis of a hepatocellular cancer.
- If you do bleed, you need to be in the care of a Monitored Environment (read, ICU) having a multi disciplinary attendance (skilled ER doctors, Intensivists, Gastroenterologists, Interventional Radiologists, etc).
What is Ascites?
Ascites means gathering fluid in the abdomen. In Liver Cirrhosis, it is usually this is also associated with the development of swelling over the feet (called edema). This complication of cirrhosis may happen to 50% of patients by 10 years after cirrhosis has been diagnosed. Having ascites after cirrhosis is a bad prognostic sign; there may be a 15% chance of death in a year, and 44% in the next 5 years.
The first time ascites is diagnosed, a small sample should be removed for analysis, as in 15% of patients, the cause may not be liver cirrhosis, thus the treatment will differ. Commonly, the doctor wants to rule out Tuberculosis, pancreatitis as well as infections in the fluid (by a culture).
Treating ascites is nearly always successful
Most patients with (mild to moderate) ascites do not need to be admitted for care. Salt restriction is the mainstay of treatment, along with medication to lose salt and water in urine called diuretics. You need not restrict your water intake unless specifically told. 90% of patients with ascites should respond to salt restriction with diuretic use alone. Along with the treatment of the cause of cirrhosis, the ascites may resolve to an extent not to need treatment anymore. This is known when alcoholics stop alcohol, as well as successful treatment with immunosuppression of Auto-Immune Hepatitis and anti Virals for Chronic Hepatitis B. When you find that the ascites has dried up, your doctor will be able to reduce the dose of the diuretics, to avoid complications. While on diuretics, getting cramps, salt disturbances (high or low sodium/potassium), behavioural changes (encephalopathy) or enlargement of breast tissue in males are considered complications needing reduction/modification of the drugs.
Advice on “salt in diet” is confusing.
Your daily salt intake should not exceed 5 grams a day (we thus allow a little more than 1 gram in each of your 3 meals). All websites and books will tell you this means “no added salt to cooked food”. However, Indian food has a lot of salt added to it during cooking (a restaurant meal could have even 10 grams of salt in a single meal!). the person who cooks the meals at home will need to be counselled about this.
But it is a serious complication of liver cirrhosis.
All patients with ascites will now remain on diuretics (medication to increase the formation of urine, thus losing the excess fluid). This means the kidneys will be under pressure to work harder. Any patient with cirrhosis getting ascites should thus consider evaluation for a liver transplant when ascites is diagnosed, as the results of transplant after the onset of kidney dysfunction are worse. If the transplant is done soon after ascites is first seen, the survival is 85% at 1 year & 76% at 3 years, nearly the same as that if going for transplant without ascites. Factors like Los sodium, low mean BP, kidney dysfunction and advancing liver disease affect the survival for surgery later.
How much ascites do I have, the doctor’s terms are confusing.
At your first contact with the doctor, he will recognize your ascites by grades: grade 1 means “seen on ultrasound only”, grade 2 means an “obvious visible distension of the abdomen”; and grade 3 is a “large protuberant belly filled with fluid”. When he is treating you; he will use the terms: diuretic sensitive (gone on medication), diuretic refractory (fluid not drying up even on a full dose medication); or, diuretic intractable 9cannot be given anymore diuretics as you are getting complications of medication.
When will the doctor say the ascites too has got “complicated”?
In case the ascites stops responding to diuretics (refractory ascites), you get infection in the fluid (SBP), your sodium drops to serious levels (hyponatremia) or you get hepatorenal syndrome (HRS); your doctor is clearly worried. All these mean you will need to be hospitalized for at least 5 to 10 days for treatment. You may need medication like IV Terlipressin and IV Albumin, each of which cost between Rs. 6,000 to 10,000 a day. You will need skilled care (often in the ICU) to recover. Unrecognized or left untreated, the mortality could rise to even 90%. Even after treatment there is a 30% and 50% chance of mortality in the first and second year (sometimes 50% in 6 months) after surviving such a complication, so you should consider transplantation soon.
Hepatocellular carcinoma
The annual risk of development of HCC in cirrhosis with Hepatitis B is 3-8%, and with Hepatitis C is 1-7%.
A sudden deterioration of liver function, unexplained weight loss or fever, jaundice or portal vein thrombosis may suggest a need to look for a HCC.
Surveillance is the repeated application of screening test/s with the aim to detect a HCC in an early stage. Early detection followed by prompt treatment has a survival benefit. From the estimated tumor growth rate, surveillance for HCC should be done every 6 months , using a combination of ultrasound of the liver and a blood test (alfa fetoprotein), to have a 90% sensitivity without a loss of specificity. If a suspicious nodule is seen, confirmation is done by a dynamic 4 phase CT liver or a Contrast (Gadoxetic acid) enhanced Liver MRI. Both can conclusively recognize that a nodule up to 2 cm wide is a tumor. For suspicious smaller nodules, repeating the tests within 3 months may confirm or rule out a tumor.
If a small tumor is confirmed in a person with a good liver function, no portal hypertension and a good performance status, he can be offered surgical resection or local ablative treatment like RFA (radiofrequency ablation). Patient s where multiple small tumors are detected simultaneously, cure could be offered with a liver transplant; as there is a higher rate of recurrence in the remnant liver after resection alone. .
Day-to-day living with Liver Cirrhosis
In liver cirrhosis, you may have a few or more restrictions on the life style. Liver cirrhosis can broadly be divided into the following groups for life style management. Your doctor may tell you which of these groups you fit into.
- Compensated cirrhosis without weight loss. (Least restrictions on lifestyle; all that are given below).
- Compensated cirrhosis with weight loss. The liver is responsible to make your protein, thus provide for muscles. As the disease advances, you may find you have lost between 6-10 kg weight; making you look “skinny”. That means your muscles have got thin (atrophic; the doctor calls this” sarcopenia”). You will need as much protein in diet as the doctor will allow safely, and remember to exercise regularly so you maintain muscle, and if possible build some more.
- Decompensated cirrhosis. This means you have now become prone to some complication of liver cirrhosis. The lifestly restrictions will be in addition to those mentioned here; your doctor will help give you this customized additional advice.
- End-stage- liver disease. This means you are very prone to complications, with a risk that you may need frequent admission to hospital for care. Here any variation from lifestyle restriction may make you prone to serious complications of liver cirrhosis. Medical management will be more important that these lifestyle restrictions alone.
Sleep early; develop a schedule for the day. You will thus be able to pick up minor changes in your health easily. A bath before bed will help get you good sleep. Getting exercise will also make you tired to generate sleep. Let your doctor know if your sleep is not restful.
Note the time you wake up daily. Changes in this will alert you about health changes.
Develop a morning routine.
- You should have 2 semi formed motions a day (not one, not formed –stools should spread on passage and not keep shape (semi formed) but should not be loose or watery. A good motion helps loose toxins that may get reabsorbed back, and the liver may have to rework to remove them.
- Measure the urine every time you pass in a measuring urine pot. Note this and total the volume for everyday. If you notice a fall in the daily urine output, you may pick up a problem before it needs you to be hospitalized.
- Then, have your bath. Cirrhotic patients who need diuretic (medicine to increase urine) will find lying in a tub improves urine output without medication. Textbooks of Medicine recognize this as “head-out immersion”.
- Use a soft toothbrush and an electric razor (it minimizes bleeding if you have a cut).
- After your bath, weigh yourself daily on your own bathroom scale. Again, this daily record of a rising weight by grams, with a falling urine output will alert you and your doctor that something could be going wrong. You may then weigh yourself in the evening again before dinner. A serial weight gain over 3-5 days needs to be reported to your doctor.
What should you eat? The broad guidelines are as follows:
- Get into the habit of eating fresh home-cooked food Food brought in from take-away or supermarket invariably has added salt, or some content that may be beyond what your liver can handle, making control of symptoms difficult for your doctor. Persons with cirrhosis who have a lifestyle of socializing end up needing more medication, more visits for adjusting doses, and are still not happy with the result. Remember, you are teaming up with your doctor to beat the condition; he cannot do it alone.
- Eat food fresh. Chances of catching a infection are higher if the food is stale or inadequately reheated. Raw foods like salads and fruit need to be washed well and cut just before consumption.
- The meals should be at regular intervals, do not miss and avoid delays. Food you eat provides for nutrition to the body immediately after; but this will last for about 4 hours. After that, the liver needs to provide for the falling blood sugar from its reserves. Some seriously ill cirrhotic patients are advised to be woken for a glass of fruit juice at 2 am too. Thus, allow your liver to retain its stores. You meal should contain a share of protein, carbohydrate as well as fat; besides vitamins and minerals. Your doctor can guide you to a dietitian for planning this.
- Do not miss food fiber. Eat a good share of salads and fruit. Fiber helps keep the intestinal bacteria healthy, and ensures a good stool.
You should know the difference between vegetarian protein and non vegetarian. Pulses, paneer (cottage cheese), daals and to some extent cereals contain vegetarian protein. This is usually safe for all cirrhotic patients. Make sure you provide for it. Meat, chicken, pork and beef are non vegetarian sources, and are the first protein to be restricted if you develop encephalopathy. In case your doctor has restricted animal protein, he will need to run some tests before allowing animal protein again. Eggs are allowed in case your doctor says so.
Cirrhotics who gain weight suddenly due to not making enough urine are getting a complication called ascites. You will then need to follow “Salt free diet with top salt” given elsewhere in this website.
Timings of drugs:
Diuretics (medicine that makes more urine): Loop diuretics (Frusemide – Lasix, Dytor, etc) work for a short span of 4-6 hours. At this time your kidneys should be getting the major share of blood supply. If at this time, you are walking around, the body needs to supply blood to your muscles preferentially, because you have asked for it. You will find your drug works less on this day. Arrange the time of the drug such that you are then sitting quietly reading a newspaper, or working at the desk. Other diuretics work 24/7; they will not be affected by this.
Exercise: if a person having cirrhosis does not exercise, the following complications will come in faster. However, avoid contact sports in case there is a risk of bleeding due to clotting disorders if the liver.
Sarcopenia: the muscles not in use will gradually become difficult to maintain. Any illness that restricts a person to bed will result in 4-5 kg of a muscle loss. Following recovery from the illness, you may suddenly find you are not able to maintain you balance as good as 2 weeks ago. And you may find it difficult to regain this lost muscle as you liver does not work fast enough. You have suddenly become an increased risk for falls and fractures. All because you did not push yourself when you suffered a common cold!
Osteoporosis: Low-Impact exercise like walking for 30 minutes a day is good enough to remind your weight bearing bones, that they are still in use and should not loose calcium, which is common in idle people. This is more so, as the liver participates in control of the steroids and vitamin D that control bone metabolism.
Alcohol: any amount of any alcohol will accelerate your liver cirrhosis, avoid completely.
Tobacco: this is a co-factor in maintaining disease as well as a carcinogen.
Sedatives: Do not use unsupervised sedatives. Tell your doctor you cannot sleep. The liver may not continue to handle the drug as well as before. You may be groggy if you wake at night, and going to the toilet may have an increased fall risk. Patients using medication for depression and anxiety will need their drugs changed by their psychiatrist, and are strongly advised to consider non medication means of managing their psychological disorder (like Cognitive Behavioural Therapy, exercise, etc).
Warning signs that should tell you to inform you doctor:
- Serial weight gain over 4-5 days.
- Black colored stools, even on one occasion; especially when also loose (keep a small clean glass bottle in the toilet so you can immediately collect that sample and send it to the Lab for “Occult Blood” testing.)
- Change in sleep pattern: staying awake at night, and sleeping through the day.
- Irrelevant behavior, inappropriate answers to questions.
- Getting tired earlier than before of late.
- Change in the taste of food, aversion, loss of appetite.
Will other medicines harm a cirrhotic liver?
The liver is an immune organ; it removes bacteria from the blood stream. A cirrhotic liver is associated with a weaked defence, and there could be as much as 5-7 fold increase in bacteria in the bloodstream. We obviously need to give antibiotics, then! But a weakened liver may have issues removing drugs from the blood too, and it does happen that usually normal doses of some drugs are harmful to a cirrhotic liver.
Are you stuck between the Devil and the Deep Sea? Not really. Most drugs can be used safely in cirrhosis, including those that are potentially hepatotoxic, but lower doses or reduced dosing frequency is often recommended, due to altered PKs. Drugs that can precipitate complications should be identified and avoided.
What is different in a person with liver cirrhosis, is that
- Other drugs may need dose modification
- May need a closer and stricter follow up
- Dugs could be competing to leave the liver through the same pathway
- Poor nutrition in cirrhosis reduces the “master trucker” molecule carrying drugs, serum albumin
- Other organs are at risk of damage, just because a drug was used when there is cirrhosis (kidney damage with painkillers, bone marrow with chloramphenicol).
- A commonly used drug may cause Liver Failure just because the liver is now cirrhotic.
So, if you have pain in abdomen, nausea or notice jaundice when you have started using a new drug, stop it and consult immediately. Better, check before starting the drug whether it has a known issue in cirrhotics. Obviously, you will need to know your CTP score, as the risks increase with increasing score.
Pain medication:
Anyone planning to go for a liver transplant should read this carefully. Patients have become unfit for transplant just because they took just one day’s dose of a risky pain killer. COX-2 inhibitor medication may lead to a massive GI bleed, precipitate encephalopathy, cause hepatorenal syndrome and also be a cause of death. Beware of names like Diclofenac (Voveran, Dynapar), Ibuprofen (Brufen, Combiflam), Naproxen (Naprosyn).
You may use Paracetamol upto 2-3 grams in a day safely for pain. If you are a CTP C class, check with me first. Oral Paracetamol 650 mg 3 times, or even 500 mg 4 times a day should be good. In case you are in the ER for an emergency, the paracetamol dose may need to be watched if a 1 gram / 100 cc bottle was used.
Oral options are Tramadol 25 mg 3 times a day. Drugs other than these (including pain relief patches) may need a doctor’s supervision, as narcotics may cause sedation.
Antibiotics:
In case you receive a prescription for any of the following drugs from another physician, you may need to let me know. The antibiotic was given to you with the best intentions, but we will need to look at the risk of using it against the severity of your liver cirrhosis. You could also check with the prescribing doctor himself, as to whether there is another option in case his first choice turns out risky for your liver.
DRUG (alphabetically) | CLASS OF DRUG | COMMONLY USED FOR |
Amikacin | Aminoglycoside | Gram negative infections |
Azithromycin | Aminoglycoside | Respiratory infections |
Augmentin | Oral penicillin | Common for infections |
Amphotercin B |
| Deep fungal infections |
Ceftazidime | Oral penicillin |
Antibiotics after admission for care |
Cefoperazone | Oral penicillin | |
Ceftriaxone | Oral penicillin | |
Chloramphenicol |
| Old antibiotic for typhoid |
Clindamycin | Aminoglycoside | Skin, soft tissue and respiratory |
Erythromycin | Aminoglycoside | Respiratory infections |
Fluconazole | Imidazole | Anti fungal |
Gentamycin | Aminoglycoside | Gram negative infections |
Gatifloxacin | Macrolide | Respiratory infections |
Griseofulvin | NOT TO USE | Antifungal |
Isoniazid |
| Anti tubercular |
Itraconazole | Imidazole | Antifungal |
Ketoconazole | Imidazole | Antifungal |
Lincomycin |
| Bone infections |
Metronidazole | Imidazole | Gut infections |
Miconazole | Imidazole | Antifungal |
Nitrofuratoin pyrazinamide |
| Urinary infections |
Nalidixic acid |
|
|
Pefloxacin | Macrolide |
|
Pyrazinamide |
| Anti tubercular |
Rifampicin |
| Anti tubercular |
Roxithromycin | Macrolide |
|
Tetracycline |
|
|
Trimethoprim sulphamethoxazole |
| Common antibiotic in general practice |
Vancomycin | Aminoglycoside | Bone, C difficile infection |
Hypertension & diabetes:
A cirrhotic due to NASH usually will also have one or all of hypertension, cardiac disease and diabetes. Very high blood pressures may need the use of Labetalol and Methyldopa, which has a high risk of liver toxicity, thus should be used only if there is no other choice. This applies to the use of Captopril, Amiodarone and Ticlopidine. The doses of commonly used antihypertensives, like ARB, ACE inhibitors & alpha blockers could need dose adjustment once cirrhosis is diagnosed. Statins are however, safe.
Many commonly used medications have issues is cirrhosis, and your doctor may just have to escalate his monitoring during use.
Anti convulsants: patients already on Phenytoin, Carbamazepine and Valproate may need a change as these can be hepatotoxic.
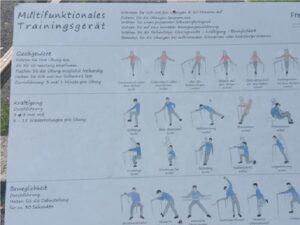
Proximal muscle exercises

While visiting my daughter in Freiburg, Germany, I found this recreational area which was designed for the elderly to get the exercise that would help maintain their muscle mass as well as the strength in their muscles of balance. It does not take much to design something for those who held our hand when we were at a “risk of fall”.
I have included a picture of the display board where various muscle groups could be worked.
Remedies as “First Aid” for common illnesses in a liver cirrhotic
Abdominal gas & bloating | Simethicone | Gelucil, Digene, Gasex tablets |
Allergies (runny nose, stuffy nose, congestion) | Diphenhydramine, Loratidine, Cetrizine (avoid those with pseudoephedrine) | Benadryl, Deslor, Cetzine |
Sneezing & runny nose | Chlorpheniramine |
|
Congestion | Guaifenesin | Mucinex |
Cough | Dextromethorphan |
|
Low grade fever , headache, joint pains | Acetaminophen (Paracetamol) Inform if fever is above 100oF | Up to 2 grams in 24 hours, Crocin 500 mg 4 times a day / Dolo 650mg 3 times a day |
Nausea | Domperidone |
|
Diarrhea | Lomotil / Imodium | If with fever & abdominal pain, notify |
|
|
|
Constipation | Polyethylene glycol Bisacodyl Senna Docusate |
|
Loss of appetite
There could be many reasons you may have lost your appetite. You would need to be assessed, but could you think of something till then? The causes of a recent loss of appetite could be varied:
- Alcohol use
- Depression
- New Liver inflammation
- Inflammation of the pancreas
- Fresh Infections
- Tuberculosis
- Cancer
- …but it may be a false alarm, too!
While you get to your doctor, what could you do to hedge the risks?
- Take note of when your appetite is best, for some people this is in the morning and appetite diminishes throughout the day. For other people it may be the opposite.
- When you feel well, eat as much nutritious food as possible in case you do not feel well later.
- Do not limit or restrict food intake when appetite is good.
Eat 5-6 small meals per day and snack anytime.
- Small amounts of food are typically easier to digest and are easier on the stomach. It is often easier to better meet nutrition needs while battling appetite loss with smaller amounts of food more frequently.
Keep healthy snacks around, and do not go more than three hours without eating.
- Keep small containers of fruit, dried fruit, trail mix, small bottles of juice, yogurt, cheese, whole grain crackers, cereal, granola bars, and other portable food items that are easy to eat and require little to no preparation.
- Always keep snacks visible and available as a reminder that it is important to eat to get the body the nutrients it needs.
- Pack a cooler or insulated lunch bag to take on longer trips or to appointments when the wait time is variable.
If food is not appealing, have a nutritious beverage instead.
- A high-protein shake or smoothie can have as many calories as a small meal or large snack.
- Have a ready-to-drink liquid nutrition supplement when food is not appealing.
- Milkshakes, smoothies, or protein shakes can be made with yogurt, milk, ice cream, protein powder, fruit, and other ingredients using a blender. Have these ingredients available for times when a drink sounds better than a meal.
Drink liquids between meals.
- Sometimes drinking liquids with meals causes the stomach to get full faster. This prevents eating enough and maximizing nutrition from food sources.
- If an early feeling of fullness is a problem, try waiting to drink any liquids until after a meal and do not drink any liquids for at least 30 minutes before a meal.
Add calories and protein to foods to give their nutrient content a boost.
- There are ways to add protein and calories to foods that are already eaten regularly.
- Add a scoop of protein powder to a shake or smoothie.
- Add healthy fat such as olive oil, nuts, or nut butter to recipes and other dishes to boost the calorie content.
- Ask a dietitian for other suggestions on how to increase the protein and calorie content of foods.
Exercise or do some physical activity at least an hour before a meal.
- Regular exercise may help increase appetite.
- Ask your healthcare team before beginning any exercise program.
- Go for a 20-minute walk before sitting down to a meal.
Get in the habit of having a bedtime snack.
- An easy-to-digest snack such as yogurt and fruit, cheese and crackers, or peanut butter and crackers is an easy way to get some additional nutrition and will not impact appetite for the next meal.
- If reflux or heartburn is an issue, have this snack at least one hour before lying down.
Emotions are often related to appetite. Talk to your healthcare team about managing your emotional well-being.
- Depression, anxiety, fear, and stress can all affect appetite.
- Get help
